Supine (laying on your back) during pregnancy
One of our Physiotherapists, Sarah, takes a look at the latest research on the recommendations for laying on your back during pregnancy
Supine exercise during pregnancy
It is widely accepted that exercise can be safe and beneficial to both mother and their baby during pregnancy, and should be encouraged in most cases. However, the physiological changes that occur during pregnancy have an effect on the way pregnant women are able to exercise safely.
There is an emerging body of evidence related to the supine position (lying on your back) while pregnant. As the weight of the uterus increases, there is more aortocaval compression (pressure on the arteries and veins) when lying on your back, which can lead to decreased blood flow to and from the heart (Spring, 2018).
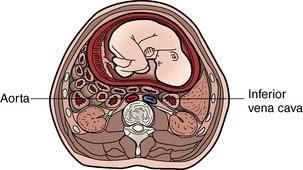

A recent study investigated the foetal response to short bouts (30 minutes) of supine lying in healthy, late gestation pregnancies (Stone et al., 2017). They found that foetuses adopted a less active state in supine lying compared with any other position, which they suggest could be an adaptive response to a decreased oxygen supply. There is also evidence that uterine blood flow decreases 13-34% in supine compared to left side-lying (Mottola, 2019; Spring, 2018).
Sleeping on your back is now considered in the “triple risk model for stillbirth” meaning that repeated, prolonged supine sleeping is regarded as a physiological stressor to the foetus and can be potentially fatal in combination with other stillbirth risk factors (Warland, 2017). These risk factors include:
Maternal risk factors such as pre-existing heart disease, restrictive lung disease, any medical condition that causes hypoxia or low blood pressure, women who smoke or have a high BMI, or women who have undergone multiple pregnancies and foetal risk factors such as intrauterine growth restriction, reduced foetal movements, or a history of being small for gestational age.
There is growing research and evidence that even if the mother is not feeling symptoms there can still be an effect on the baby and for this reason, we strongly advise women at our clinic to commence prenatal Pilates after the first trimester (13 weeks). Unlike regular reformer Pilates, prenatal Pilates is modified to avoid prolonged bouts of supine lying and is led by physiotherapists trained in prenatal exercise. This also allows us to screen for risk factors that could contraindicate specific exercises, pick up on symptoms of aortocaval compression, and manage pregnancy related pain during exercise.
If you are approaching your second trimester of pregnancy or have any of the aforementioned risk factors and want to continue exercising safely, speak with us about prenatal Pilates!
Humphries et al, 2020 https://pubmed.ncbi.nlm.nih.gov/31856296/
Mottola, 2019: https://bjsm.bmj.com/content/53/2/82.long
RANZCOG guidelines: https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Exercise-during-pregnancy-(C-Obs-62).pdf?ext=.pdf
Spring, 2018: https://pogp.csp.org.uk/sites/default/files/journal/2018-08/15_14301043.pdf
Stone, 2017: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5309385/
Warland, 2017:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5309362/